Gastric Bypass
A Restrictive and Malabsorptive Procedure
What is Gastric Bypass?
Gastric bypass is a restrictive and hormonal procedure that alters the digestive system to reduce hunger by modifying hormone levels. It increases hormones that promote fullness while decreasing those that cause hunger. This adjustment leads to reduced appetite and early satiety (feeling full after just a few bites), resulting in lower food intake and significant weight loss.
Beyond weight loss, gastric bypass surgery has a powerful metabolic effect, particularly in managing type 2 diabetes. Many patients achieve diabetes remission, with normal blood glucose levels and reduced or eliminated need for medication. In the first few years after surgery, patients typically lose about 60% or more of their excess weight. For lasting success, adopting new eating habits and maintaining a low-calorie diet is essential.
How Does Gastric Bypass Work?

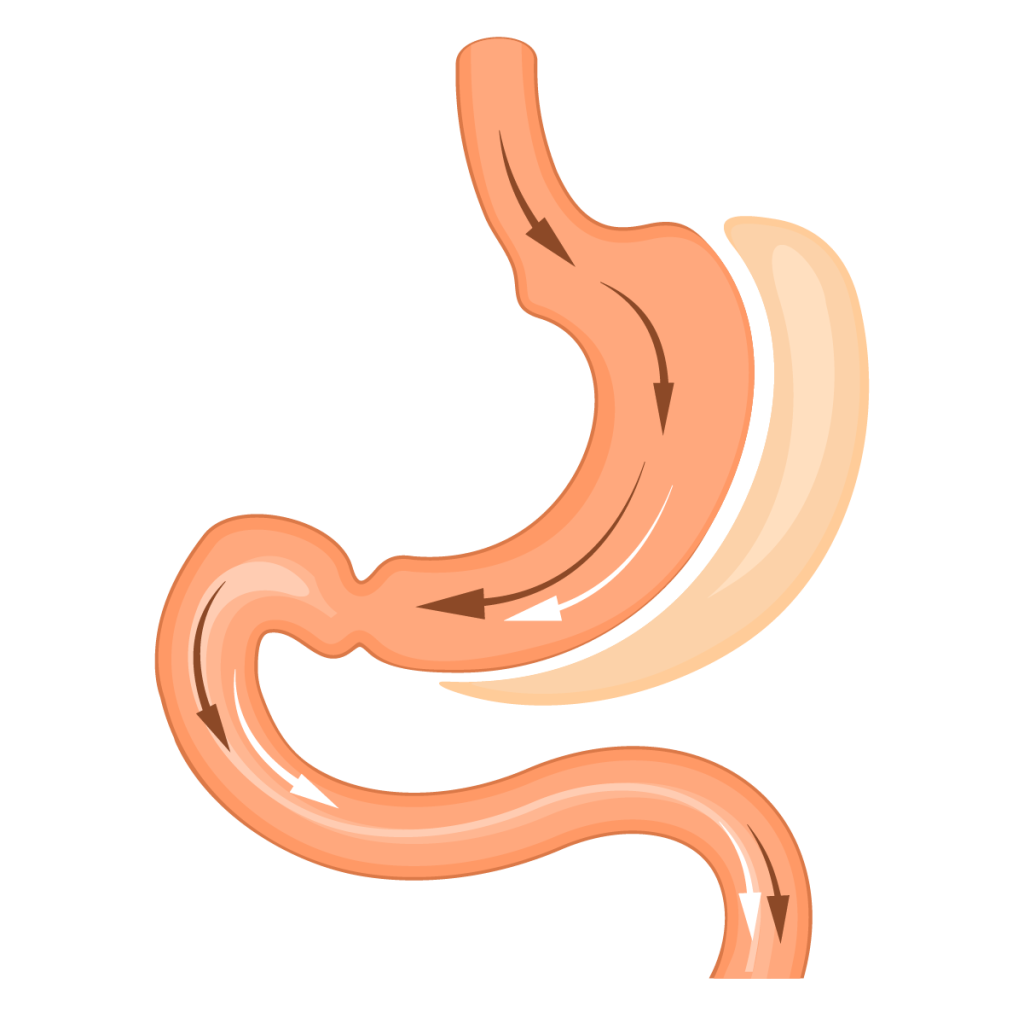
The surgery involves creating a small gastric pouch (roughly the size of a coffee cup) that holds only a small amount of food. This pouch is completely separated from the rest of the stomach and is connected directly to a segment of the small intestine. While food bypasses the majority of the stomach, the stomach itself remains intact.
By bypassing the stomach and the initial sections of the small intestine (the duodenum and proximal jejunum), the procedure can lead to decreased absorption of certain vitamins and minerals. As a result, patients need to take supplements like multivitamins, calcium, and iron to maintain adequate levels.
Benefits of Gastric Bypass
Gastric bypass surgery offers multiple benefits:
- Reduces food intake by curbing hunger and accelerating the sensation of fullness.
- Average weight loss is around 60% of excess weight, with effective long-term maintenance, especially in patients with a BMI below 50.
- Particularly effective for type 2 diabetes, normalizing blood sugar and hemoglobin A1c levels in approximately 80% of cases.
- Helps alleviate gastroesophageal reflux disease (GERD) symptoms.
However, patients with a BMI above 50 may experience less weight loss, and 40% may face challenges in long-term weight maintenance.
What Are the Potential Complications?
Like any surgical procedure, gastric bypass surgery comes with potential risks, including:
- Nutrient deficiencies, such as iron, vitamin B12, or folic acid anemia
- Calcium deficiency, which can lead to osteoporosis
- Intestinal obstruction (e.g., volvulus, internal hernia)
- Dumping syndrome, causing hypoglycemic episodes after eating
- Acute vitamin deficiencies due to persistent vomiting
Who Can Benefit from Gastric Bypass?
Gastric bypass is ideal for individuals with long-standing type 2 diabetes, especially those requiring insulin therapy. It is also effective for those suffering from severe gastroesophageal reflux disease (GERD). Additionally, it is a recommended revision surgery for patients who have had gastric banding but did not achieve sufficient weight loss.
Follow-Up Visits
Regular follow-up appointments are crucial to optimize weight loss and manage potential issues like nutrient deficiencies or dumping syndrome. Patients must maintain a supplement regimen, including iron, vitamins, and occasionally calcium.
Preparation Requirements
Before undergoing gastric bypass, patients need to have an endoscopic examination of the esophagus, stomach, and duodenum to ensure there are no underlying conditions that might affect the surgery.
Bariatric and Metabolic Surgery
Surgical treatment of patients with morbid obesity
Sleeve gastrectomy


